Zhangjiagang Bailing Specimen Model Co., Ltd.
Contact:Mr Zhang
Eelephone:13506223680
Eelephone:18962473680
E-mail:cnbbmx@163.com
605340177@qq.com
Website:www.cnbbmx.com
Address:Bridge No. 4, Leyu Town, Zhangjiagang City, Suzhou City
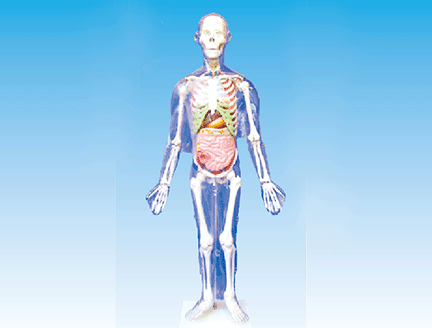
Human Body Model - Interference of Physiological Function by Artificial Ventilator
Artificial ventilation with an artificial ventilator is not exactly the same as spontaneous breathing, or even completely different. It has positive and negative effects on physiological functions. It goes without saying that artificial ventilation has beneficial effects on physiology, and a full understanding of artificial ventilation Physiological interference with rational selection and correct use. Artificial ventilator is of great significance to improve treatment effect and reduce complications.
(1) Interference to breathing physiology. Under normal physiological conditions, the pressure in the airway, alveoli and thoracic cavity is basically below atmospheric pressure, and may be higher than atmospheric pressure only at the beginning of expiratory phase. The magnitude is not large, which is undoubtedly beneficial to maintain normal venous blood return to the heart and cardiac output. Artificial ventilation, especially positive pressure ventilation and high-frequency ventilation, in the inspiratory phase of the breathing cycle, the airway, alveolar and intrathoracic pressures are significantly higher than atmospheric pressure. If the airway pressure is greater than 2.942kPa, it may lead to the destruction of lung tissue and interstitial structure. . Mediastinal, subcutaneous emphysema or pneumothorax occurs, causing barotrauma. Positive airway pressure can dilate airways and alveoli, increase lung gas capacity, improve gas exchange, and also increase anatomical dead space. The increase or decrease of physiological dead space also depends on the impact of positive intrathoracic pressure on pulmonary blood flow. Spontaneous breathing relies on the expansion and contraction of the thorax to complete ventilation. Therefore, the alveolar ventilation and ventilation around the lungs of the simulated human lung are better than those in the central peribronchial lung tissue. Self-respiration, the body can adjust its own inspiratory force and ventilation according to physiological functions and metabolic needs. On the contrary, positive pressure ventilation makes the central alveoli expand better, and the gas exchange site is mainly located in the alveoli at the alveolar duct. Due to changes in ventilation mechanics and the characteristics of gas rheology, positive pressure ventilation can also cause uneven distribution of gas in the lungs. The length of inspiratory time affects the distribution of gas in the lungs. If it is too short, it will increase the uneven distribution, and if it is too long, it will increase the interference to the circulation. Clinically, it should be adjusted according to the specific situation. In spontaneous breathing, gas enters the lungs during inhalation, and the blood flow in the lungs also increases, accounting for about 9% of the total blood volume. When the gas is exhaled, the pulmonary blood volume drops to 6% of the total blood volume. During positive pressure ventilation, the gas in the inspiratory phase enters the lungs, but the pulmonary blood vessels are compressed, forcing the pulmonary blood to transfer to the abdominal cavity and surrounding blood vessels. When the inspiratory pressure reaches 2.942kPa, 50% (about 500mL) of the spontaneously breathing pulmonary blood volume is squeezed Out of the thoracic cavity, 3% of it flows to the extremities, and 47% enters the abdominal cavity. If the vascular nerve reflex is normal, it can be compensated by systemic vasoconstriction to maintain the effective pulmonary blood volume. If hypovolemia, acidosis, hypoxia, pulmonary capillary spasm, or peripheral vasomotor disturbances are already present, the disturbance of pulmonary circulation by positive airway air is more serious. The direct effect of positive pressure ventilation on pulmonary circulation can indirectly force the proportion of ventilation blood flow in the lungs, especially when the pressure is not suitable, the airway pressure is too high, the tidal volume is too large, the inspiratory time is too long, and the ventilation blood flow ratio increases. , resulting in an ineffective space effect, and at the same time, pulmonary blood can flow to the site with poor ventilation and low alveolar pressure, increasing the pulmonary arterial and venous shunt. In addition, during artificial ventilation, there is more air supply to the apex of the lung and less blood flow, and less air to the bottom of the lung and more blood flow. The positive intrathoracic pressure of the nurse model affects the venous return, reduces the output of the right heart, and reduces the pulmonary blood flow, which can interfere with the ventilation blood flow. Proportion. Imbalanced ventilation and blood flow can also affect gas diffusion and blood oxygenation. Artificial ventilation, especially when fully supported by ventilation, can greatly reduce the work of breathing. However, if a man-machine confrontation occurs, the work of breathing can be significantly increased. Artificial ventilation improves hypoxia and relieves the respiratory excitement caused by hypoxic stimulation. If combined with over-expansion of lung capacity, the stretch receptors in the lungs are excited, which can lead to spontaneous breathing depression. Long-term artificial ventilation can also cause ventilator dependence.
(2) Interfering with circulatory function, appropriate artificial ventilation can improve cardiac insufficiency secondary to hypoxia and carbon dioxide accumulation, relieve myocardial ischemia, and facilitate the recovery of ischemic heart disease. The intrathoracic pressure changes the circulatory law in the physiological state. When breathing spontaneously, the intrathoracic pressure decreases during inspiratory phase, and the central vein is expanded by the tracheal intubation training model, the return blood volume increases, the right heart output also increases, the pulmonary capillaries expand, the vascular resistance decreases, and the right heart afterload decreases. Conducive to further strengthening the right ventricular output function. During exhalation, the pulmonary blood vessels are squeezed, and a large amount of blood quickly returns to the left heart, which increases the output of the left heart. Therefore, spontaneous breathing plays a role in assisting circulation, while positive pressure ventilation compresses the central veins and lungs during the entire inhalation process. The vascular bed reduces both venous blood flow and cardiac output, especially the right ventricular output decreases significantly, and the left ventricular output also decreases significantly over time, resulting in coronary ischemia and weakened myocardial contractility, forming a vicious circle. Increased airway pressure, prolonged inspiratory time, increased inspiratory-to-expiratory ratio, increased respiratory rate, and positive end-expiratory pressure (artificial or spontaneous) are all important factors affecting return to the heart and cardiac output. It can aggravate the disturbance of circulatory function. It is generally believed that when the airway pressure reaches 2.942kPa, the venous return to the heart blood volume is significantly reduced. Such as adding a 2:1 ratio of breathing can reduce cardiac output by 33%, and positive pressure ventilation also increases central venous pressure (CVP).
(3) Interference to cerebral blood flow (CBF) and intracranial pressure (ICP), the main interference of artificial ventilation is the reduction of CBF, the obstruction of intracranial venous return and the increase of ICP, which depends on the management of artificial ventilation. CBF is largely regulated by arterial carbon dioxide partial pressure, which increases arterial carbon dioxide partial pressure, intracranial vasodilation, decreases vascular resistance, increases CBF, and increases ICP. The opposite effect occurs when the partial pressure of carbon dioxide in the arterial blood decreases. Artificial ventilation can reduce the partial pressure of carbon dioxide in the arterial blood and reduce the CBF. If the partial pressure of carbon dioxide in the arterial blood is lower than 2.666kPa, the CBF can be reduced by 60%, and the generation of cerebrospinal fluid is also reduced, so the ICP is reduced. Neurological symptoms caused by elevated blood carbon dioxide pressure are very effective, and hyperventilation is also effective in reducing ICP elevations of all causes. However, during hyperventilation, such as high airway pressure, positive intrathoracic pressure (especially end-expiratory positive intrathoracic pressure) prevents venous return, affects the return of intracranial blood to the heart, and can reduce CBF and increase 1CP. Therefore, in patients with traumatic brain injury and cerebral edema, the airway pressure of artificial ventilation should be properly controlled, and PEEP should not be used as much as possible, and it should not be greater than 490.3Pa when it must be used. beneficial.
(4) Interference with renal function, artificial ventilation can reduce renal blood flow, urine output, and water and sodium retention. The main influencing mechanisms are: 1. Due to the interference of positive pressure ventilation on circulatory function, resulting in decreased blood perfusion and renal vein Increased blood pressure reduces renal blood flow and is accompanied by redistribution of blood within the kidneys, ultimately leading to decreased renal function. 2. Positive pressure ventilation reduces cardiac output, increases sympathetic nerve activity, and increases catecholamine secretion. Because renal blood vessels are very sensitive to catecholamines, renal vasoconstriction increases blood flow reduction. 3. Systemic and hemodynamic changes increase plasma levels of antidiuretic hormone, renin, angiotensin, and aldosterone through various mechanisms, thereby reducing urine production and excretion. (5) Other disturbances, artificial positive pressure ventilation also has the following physiological disturbances: 1. Central venous return is blocked; it can cause liver congestion and liver ischemia, resulting in liver swelling and liver function damage. 2. Inferior vena cava congestion, gastrointestinal vascular congestion, portal hypertension, combined with gastrointestinal stress ulcers caused by primary disease or artificial ventilation, and finally gastrointestinal bleeding can occur.

Eelephone:13506223680 landline:0512-58961302
fax:0512-58961302 Website:www.cnbbmx.com
Address:Bridge No. 4, Leyu Town, Zhangjiagang City, Suzhou City
|
| |
cell phone station | WeChat public account |

